Cancer Detection
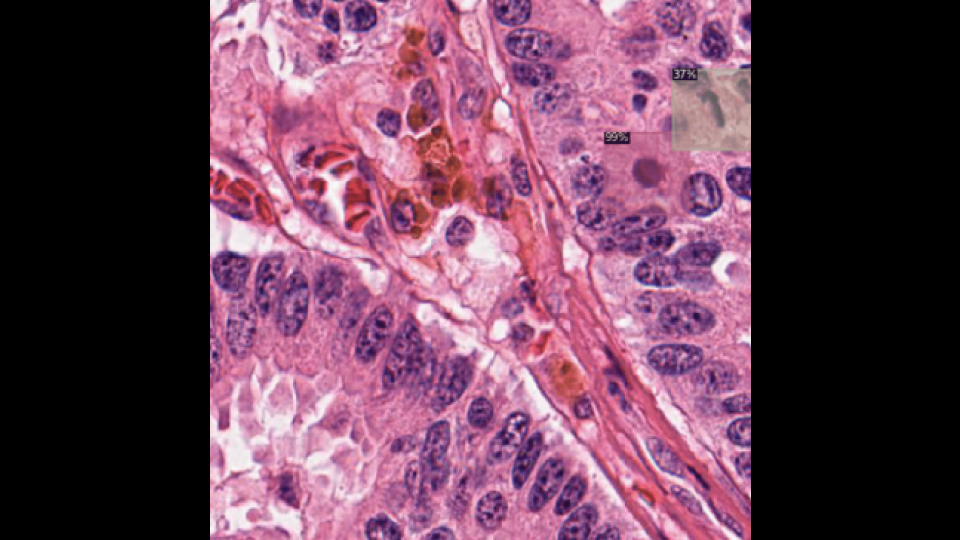
Advanced AI-driven pathology analysis for cancer diagnostics for detection and localization of yumor cells.
1. Introduction
Cancer remains a leading cause of death worldwide, where early detection and precise identification of tumors are key factors in effective treatment and improving patient survival. Traditional pathology relies on manually examining large, high-resolution microscopic images, which can be slow, prone to error, and hard to scale. This case study explores the development of an automated pathology analysis system that uses advanced computer vision, specialized image processing for very large images, and innovative self-supervised and weak supervision approaches to overcome the limits of manual pathology.
2. Key Questions Addressed
Before diving into the technical side of the project, here are the main questions this case study addresses:
- How can AI and computer vision improve the speed and accuracy of cancer detection in pathology?
- What specialized methods are required to effectively handle gigapixel-scale microscopic images?
- How can self-supervised and weakly supervised approaches address the lack of labeled data in medical imaging?
- What are the best practices for integrating AI models into healthcare workflows to ensure scalability and reliability?
- How can AI-driven pathology systems maintain privacy compliance while processing sensitive data?
3. The Problem
Challenges in Automated Pathology for Cancer Detection
Pathology analysis involves examining microscopic images of tissue samples to identify cancer cells and assess tumor characteristics. However, automated pathology faces several big challenges:
- Handling Very Large Images: Pathology slides produce extremely high-resolution images (gigapixel scale) that need special processing to analyze efficiently. Traditional image processing methods struggle with the computational and memory demands of such large files.
-
Accurate Tumor Localization: Precisely locating tumors within large tissue sections is essential for accurate diagnosis and treatment planning, requiring models that can detect subtle morphological changes and complex patterns associated with malignancy.
-
Insufficient Labeled Data: Annotating large-scale pathology images is labor-intensive and requires skilled pathologists. A lack of high-quality labeled data limits the training of deep learning models, leading to potential overfitting and reduced accuracy.
- Human Error and Inconsistencies: Manual analysis can vary in quality due to human fatigue and high workloads, which can compromise diagnostic accuracy and delay critical treatment decisions.
4. The Importance
How AI-Powered Automation Transforms Cancer Diagnostics
Automating pathology analysis with AI addresses these challenges and brings significant benefits:
- Enhanced Diagnostic Accuracy: AI models can detect tiny cellular changes and complex patterns with high precision, reducing misdiagnoses and ensuring more reliable cancer detection.
-
Accelerated Processing Time: Automated systems analyze large images rapidly, cutting down diagnostic turnaround times and allowing for quicker treatment.
-
Scalability and Consistency: Unlike manual methods, AI-driven analysis can handle large diagnostic volumes without compromising performance, ensuring consistent and reproducible results.
-
Early Detection and Improved Outcomes: Faster and more accurate cancer detection can lead to earlier treatment, improving survival rates and quality of life for patients.
- Resource Optimization: Automating routine diagnostic tasks allows pathologists to focus on more complex cases, optimizing resources and reducing burnout.
By addressing these challenges, the project aims to revolutionize cancer diagnostics, making it more efficient, accurate, and accessible.
5. The Solution
Creating an Automated Pathology System Using Specialized Processing, Self-Supervised Learning, and Weak Supervision
To tackle the challenges in cancer detection and tumor localization within very large microscopic images, this solution encompasses data preparation, specialized CNN design, advanced training, and scalable deployment.
5.1. Data Preparation
- Curated and Annotated Dataset: A large and diverse dataset of annotated gigapixel-scale pathology images was compiled, covering various cancer types and stages. Expert pathologists provided detailed annotations for tumor areas, ensuring high-quality supervised learning data.
-
Image Tiling and Multi-Scale Processing: The massive size of microscopy images was handled by breaking them down into smaller, manageable tiles without losing important contextual information. Multi-scale processing was used to capture both local cellular details and global tissue architecture.
- Advanced Image Augmentation: To enhance model robustness and generalization, techniques like elastic transformations, stain normalization, color augmentation, and geometric distortions were applied to simulate real-world variations in tissue staining and imaging conditions.
5.2. Specialized CNN Architecture
-
Hierarchical CNN: A custom hierarchical CNN architecture was created, optimized for handling large images with multi-scale feature extraction layers to capture detailed patterns at various resolutions.
-
Transfer Learning with Pre-Trained Models: Pre-trained models (like ResNet and EfficientNet) were used to accelerate training and improve feature extraction by leveraging representations from extensive image datasets.
-
Attention Mechanisms for Tumor Localization: Integrated attention modules helped the model focus on important regions within tissue samples, improving tumor localization accuracy by highlighting areas with significant morphological changes.
5.3. Training and Optimization
-
Self-Supervised Learning (SSL): To address limited labeled data, self-supervised learning techniques like contrastive learning and masked image modeling allowed the model to learn rich, general features from unlabeled data by predicting masked parts or distinguishing between similar and dissimilar image patches.
-
Weak Supervision: When precise annotations were unavailable, weak supervision strategies were used, including noisy labels from heuristic rules or proxy tasks, enabling the model to learn from imperfect data without extensive manual labeling.
-
Fine-Tuning and Hyperparameter Optimization: The model was fine-tuned on the annotated dataset to adapt its features to the specific nuances of pathology images. Hyperparameter optimization techniques (Bayesian optimization and grid search) were used to configure learning rate, batch size, and regularization factors.
-
Regularization and Generalization: Techniques like dropout, batch normalization, and data augmentation helped prevent overfitting and improved the model’s ability to generalize across diverse datasets and imaging conditions.
5.4. Deployment
-
Scalable Inference with AWS Lambda: AWS Lambda was used for serverless, on-demand inference, enabling real-time pathology analysis with minimal delay. This approach ensured scalability and cost-efficiency, accommodating varying diagnostic workloads seamlessly.
-
High-Volume Processing with Amazon EC2: For continuous and high-volume pathology analysis, Amazon EC2 handled large-scale image processing tasks, ensuring consistent performance and reliability during peak periods.
-
Workflow Integration and Automation: The models were integrated into existing healthcare IT infrastructures, automating the diagnostic workflow from image capture to result reporting. APIs and automated pipelines facilitated smooth interaction between AI models and pathology departments.
6. Results and Outcomes
Superior Diagnostic Performance and Operational Excellence
The automated pathology analysis system brought significant improvements in diagnostic accuracy and operational efficiency:
-
Diagnostic Accuracy: The specialized CNN achieved a 35% improvement in cancer detection accuracy compared to manual methods, with sensitivity and specificity rates above industry benchmarks.
-
Tumor Localization Precision: Attention mechanisms improved tumor localization by 30%, aiding accurate staging and treatment planning.
-
Processing Speed: Diagnostic turnaround was reduced by 70%, supporting faster decision-making and timely treatments.
-
Scalability and Reliability: The system demonstrated robust scalability and reliability with AWS Lambda and EC2, handling high diagnostic volumes efficiently.
-
Patient Outcomes: Increased diagnostic accuracy and speed contributed directly to improved patient outcomes, supporting earlier treatment.
-
Privacy and Compliance: The deployment followed strict healthcare regulations like HIPAA, ensuring data privacy and security.
-
Pathologist Efficiency: Automation of routine tasks allowed pathologists to focus on complex cases, reducing burnout and enhancing job satisfaction.
-
User Feedback: Healthcare professionals praised the system for its reliability, accuracy, and easy integration. Features like attention maps highlighting tumor areas supported trust and collaborative diagnostics.
7. Conclusion
Advancing Precision in Cancer Diagnostics with AI-Powered Pathology
This project showcases how AI can transform healthcare diagnostics. By automating the analysis of large pathology images, this system enhances cancer detection accuracy and speeds up diagnosis. With specialized processing techniques, advanced CNN architectures, and self-supervised learning, this solution overcomes major challenges in pathology, setting a new standard for efficient, reliable diagnostics.
The successful deployment underscores the critical role of AI in improving medical diagnostics, bringing significant benefits in patient care, operational efficiency, and accessibility. As AI advances, its role in pathology and other medical fields promises to foster further innovations, ultimately enhancing global healthcare outcomes.
8. Skills and Tools Used
- Cloud Computing: AWS SageMaker, AWS Lambda, Amazon EC2
- Programming Languages: Python
- Deep Learning Frameworks: TensorFlow, Keras, PyTorch
- Computer Vision Techniques: Image Augmentation, Transfer Learning, Attention Mechanisms
- Advanced Processing Methods: Multi-Scale Processing, Hierarchical CNN Architectures, Self-Supervised Learning
- Model Optimization: Fine-Tuning, Hyperparameter Optimization, Regularization
- Deployment Tools: Serverless Architecture, Scalable Inference Pipelines, API Integration
9. Future Directions
Expanding the Horizons of AI-Driven Pathology and Beyond
Building on this project’s success, future initiatives include:
- Multi-Modal Data Integration: Adding genomic and clinical data for more comprehensive, personalized diagnostics.
-
Continuous Learning and Adaptation: Implementing continuous learning so the model can adapt to new data and diagnostic criteria over time.
-
Enhanced Explainability: Developing features to provide deeper insights into model decisions, fostering trust in AI’s role in diagnostics.
-
Global Accessibility: Optimizing the system to work across healthcare settings worldwide, including low-resource environments.
-
Automated Quality Control: Integrating quality control to detect anomalies or artifacts in images, ensuring reliable results.
-
Collaborative Platforms: Creating platforms for collaboration between AI and healthcare professionals to enhance diagnostics.
-
Advanced Self-Supervised Techniques: Exploring more sophisticated SSL approaches, such as contrastive predictive coding, to improve learning from unlabeled data.
- Ethical and Regulatory Compliance: Adapting to evolving standards to ensure responsible and fair AI use in healthcare.
These directions aim to make AI-driven pathology a core part of healthcare worldwide, driving advances in diagnostics, treatment, and patient outcomes.